"The Cornea in WAGR Syndrome: Keeping the Window Clean"
Aniridia-associated Keratopathy is also called corneal pannus or corneal scarring. The cornea is the clear, dome-shaped covering at the front of the eye. In the normal eye, it covers the area of the pupil and the iris, and is completely clear.
Keratopathy occurs when the cornea becomes cloudy and blood vessels begin forming over it. In Aniridia, keratopathy is thought to be the result of an insufficent number of specialized cells called limbal cells. Located in an area of the eye called the Limbus, these cells help the cornea maintain its clear surface and recover from irritation or injury. Other abnormalities common in the aniridic eye, such as a condition called "dry eye," poor quality tears, and problems with the corneal nerves may also play a role in the development of keratopathy.
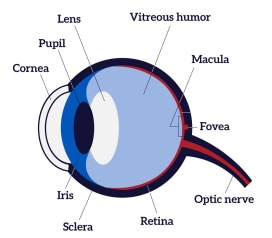
Diagram of the Eye

Normal Cornea

Aniridic Keratopathy
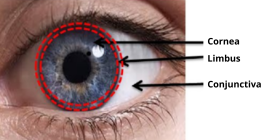
Illustration of Limbus
Any injury to the surface of the eye, such as eye infections or irritation from contact lenses, may worsen keratopathy. Eye surgery and, in some cases, treatment for glaucoma may also worsen keratopathy.
Keratopathy forms at the edges of the cornea first, then over time progresses inward toward the center of the cornea. As keratopathy progresses, vision is reduced because the cornea is no longer clear.
Keratopathy occurs in more than 90 percent of individuals with Aniridia. It often begins in the first decade of life but may not begin to affect vision until adulthood.
Development of aniridia-associated keratopathy may be unavoidable. However, the onset of this condition may be delayed or its progression slowed by:
Aniridia-associated Keratopathy is diagnosed by an eye doctor. Using a slit lamp (a high-powered microscope) the doctor can closely examine the surface of the cornea.
"Dry eye" may be the first symptom of Aniridia-associated Keratopathy. An ophthalmologist can measure the amount of moisture on the cornea, and this measurement can be an important tool for detecting and monitoring the degree of dry eye in a patient with Aniridia.
Nonsurgical treatment of Aniridia-associated Keratopathy may include:



When Aniridia-associated Keratopathy has progressed to the point that functional vision is lost, a cornea transplant may be recommended. Unfortunately, cornea transplant alone almost always results in regrowth of the keratopathy and failure of the transplant.
Success rates improve when the cornea transplant is combined with transplant of limbal stem cells. Unlike cornea transplant alone, transplant of limbal stem cells require long-term use of medication to suppress the immune system and prevent rejection of the transplanted tissue.
An alternative treatment for late-stage (light perception only) Aniridia-associated Keratopathy is the Boston Keratoprosthesis or “KPro.” This device is an artificial cornea. It may be an option for individuals who are not able to tolerate immunosuppressive drugs. The success rate for this device is low, but it is an option for those with blindness. The Boston Keratoprosthesis requires permanent use of a contact lens and antibiotic eyedrops after the procedure. Glaucoma may occur before or after KPro but can be controlled in about 80 percent of patients.
The International WAGR Syndrome Association is working to stimulate research on Aniridia.
Sign up for News & Events
COPYRIGHT© 2025 IWSA / International WAGR Syndrome Association
